Abstract

Background and Objective
The rapid spread of the COVID -19 pandemic and the high variability of the course of the disease make it essential to search for early predictors of outcome. The objective of our study is to predict severe SARS COV2 pneumonia using early cytometric profiles
Material and Methods
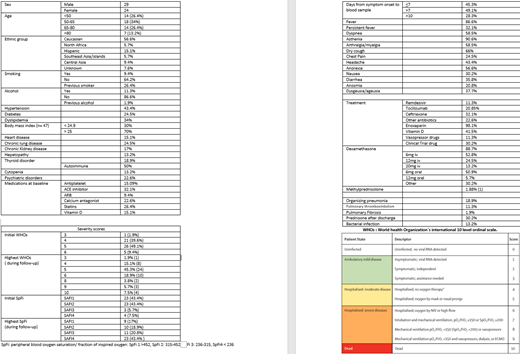
Prospective and observational study of adults with confirmed COVID-19 infection admitted on Emergency Department (ED). We collected epidemiological, clinical and laboratory data of every patient until they were discharged or died. Multiparametric flow cytometry (FC) analysis of T-lymphocytes (CD4, CD8, CD4 activated, CD8 activated, naïve (Tn), central-memory (Tcm), effector-memory (Tem), effector (Te) and Th17 subsets), B-lymphocytes (naïve, memory, transitional subsets, and assessment of clonality), NK cells, plasmablasts, p-DCs (plasmacytoid dendritic cells), m-DCs (myeloid dendritic cells), basophils, and monocytes (MO1, MO2, MO3, slan+ MO3) was performed on whole peripheral blood collected on EDTA, before immunosuppressive therapy was started. We designed a 7-tube 8-color experimental panel. Cell surface staining of 2 × 106 cells was performed and at least 500 000 total events were acquired for the assessment of plasmablasts, p-DCs, m-DCs, basophils, and the monocyte subsets; for the study of B, T and NK-lymphocyte populations we acquired at least 100 000 total events (FACS Canto II; BD Biosciences). Severity was assessed on the basis of World Health Organization´s (WHO) international 10 level ordinal scale (WHOs) and also according to 4 respiratory status, based on SpO2(peripheral blood oxygen saturation)/FIO2 (fraction of inspired oxygen) ratio (SpFi). SpFi group 1 >452, SpFi2 2: 315-452; SpFi 3 236-315, SpFi 4: <236 (respiratory distress)
Results
53 patients were included: epidemiological and clinical data available on table 1. 23 patients (43.39%) arrived to SpFi4 status. WHOs >6 (WHO 6:oxygen by non invasive ventilation or high flow) was achieved by 20 patients (37.7%)
Good prognosis (meaning SpFi1 as the worse respiratory status in the follow -up) was associated to cytometric profiles: there was a significant increase in CD3, p-DCs, m-DCs, basophils, monocytes, Tcm, % of lymphocytes and CD3/CD19 ratio whereas there was a significant reduction in CD19, % of neutrophils and % Neutrophils/% lymphocyte ratio. In the SpFi4 group, there was a significant reduction of CD3, p-DCs, m-DCs, plasmablasts and CD3/NK ratio. In patients starting in SpFi group 1-2 in the ED but progressing to SpFi 3-4 during the follow up (27 patients), there was a statistically significant relation with Tn, Te and Tn/Te ratio (Tn/Te ratio <0.717: OR 13.5 (p 0.002, [95% CI 2.552-71.403). Initial SpFi1 patients that evolved to SpFi 3-4 during follow up (10 patients), presented a Tn/Te ratio < 0.717 with an OR 11.556 (p =0.005, [95% CI 2.059-64.853]).
Plasmablasts < 0.075 and CD3/NK <5.71, were identified as independent risk factors for SpFI4 during follow up. After multivariable analysis, both variables kept their significance: CD3/NK (OR 11,247, p=0.005) and plasmablasts (OR 12,524 , p=0.004). About prediction of WHOs >6, multivariable analysis showed CD3/NK <5.71 (OR 22,240 [95%CI 2,340-211,342] p= 0.007) and plasmablasts<0.075 (OR 28.635 [95% CI 3,187-257,301] p=0.003).
A score (0,1,2) comprising both risk factors, was significantly predictive of SpFI4, regardless of the initial respiratory status, age or days from symptoms onset. In our cohort, only 1/15 (6.7%) patients with 0 points (neither plasmablasts nor CD3/NK score), arrived to SpFi4. However, 10/11 (90.9%) patients with 2 points, reached to SpFi4 respiratory status (C-index = 0.837) Same score was applied to predict WHOs > 6: 90.9% with 2 points progressed to WHO>6 and 0/15 patients with 0 points reached the same goal (C-index = 0.872)
An incidental finding of 4 indolent B-lymphoproliferative disorders (2CLL-like MBLs and 2non -CLL-like MBL), was found, and they were associated with older age and progression to death.
Conclusions
Flow cytometry on whole peripheral blood samples of SARS-COV2 pneumonia patients, collected before corticosteroid or immunosuppressive therapy, could identify cytometric patterns associated to prognosis. Plasmablasts, mDCs and pDCs levels as well as CD3/NK ratio, are associated to a worse respiratory status, while Tn/Te ratio could detect non-severe patients who will require high-flow oxygen devices during follow up.
No relevant conflicts of interest to declare.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal